Does cancer care about sex?
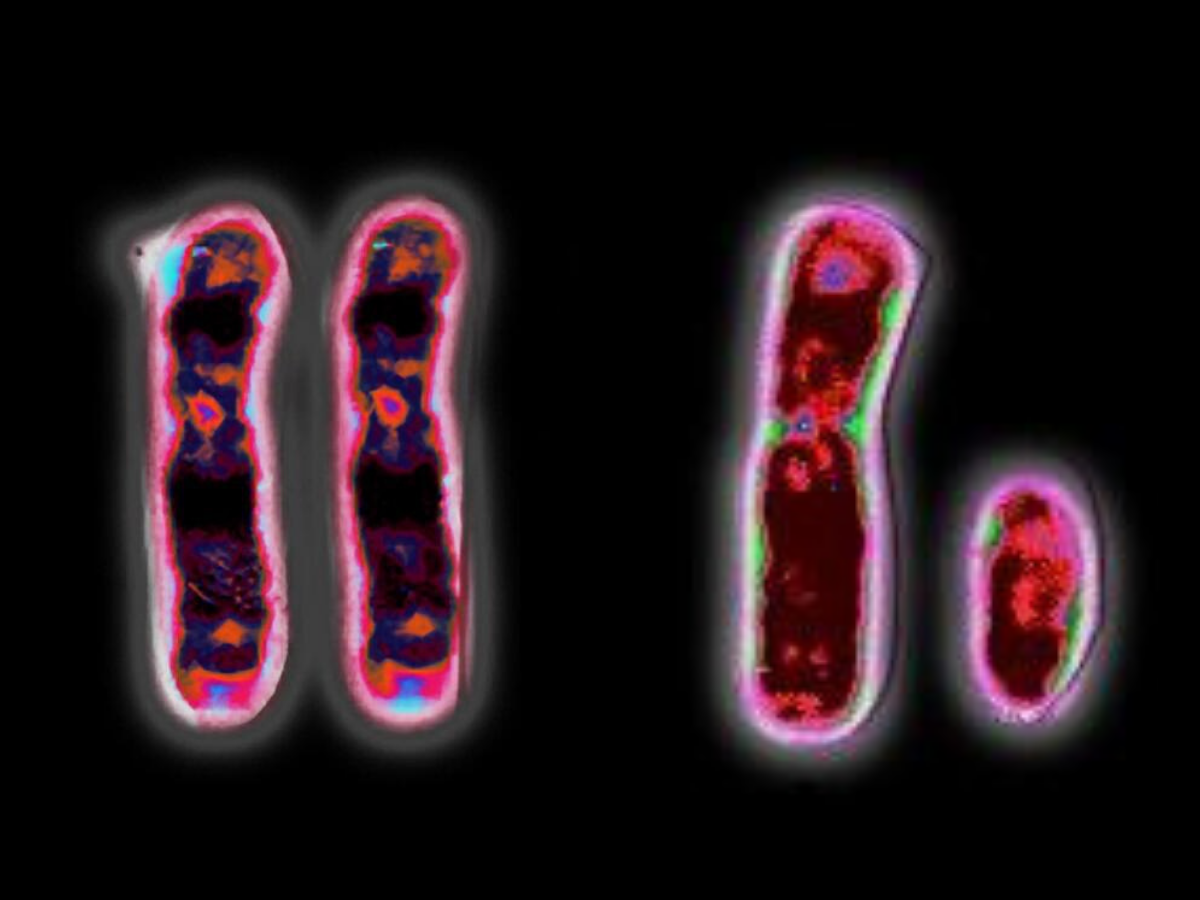
XX and XY chromosomes. Image credit: Wessex Reg. Genetics Centre
"Click here to listen to the full podcast episode"
Our second tale today also comes from one of the other fascinating sex-related stories I uncovered while researching my book Rebel Cell. Now, it’s obvious that there are differences in anatomy between humans that affect our chances of getting certain types of cancer. If you’ve got a cervix you can get cervical cancer, whatever your gender identity. If you don't, then you can’t. The same goes for ovaries, wombs, testicles and prostate glands. And although men have a greater risk of cancer overall, there are discrepancies in the incidence of cancers affecting both sexes. For example, breast cancer is overwhelmingly a female disease, with around 55,000 women diagnosed every year in the UK compared with around 350 men. Oesophageal cancer is twice as common in males than females. Now, while some of this may be down to hormones or health habits, such as smoking, diet and drinking alcohol, it’s not enough to explain all the differences.
It's increasingly becoming clear that another reason could be the sex chromosomes themselves. Genetically speaking, people who have two X chromosomes are female while those with an X and a Y are male. The Y has only a tenth as many genes as the X, is around a third of the size of the X and has a habit of accidentally going missing when cells divide. Y chromosomes have been reported missing in the blood cells of older men, especially those who smoke, and this seems to be linked to a higher risk of various types of cancer. But, as Professor Kristin Swanson discovered, there are some even more fundamental differences when it comes to the sex of cancer cells, and how they behave in the body.
A mathematician by training, Kristin Swanson is an unconventional professor of neurosurgery at the Mayo Clinic in Phoenix, Arizona, wielding equations with the same skill and precision that her surgical colleagues wield their scalpels. Over the past fifteen years she’s been building a database of thousands of patients with brain tumours, scraping every pixel of data from their MRI scans to build mathematical models that can help to predict how their cancers will grow and the best option for treatment.
For a start, Swanson’s data backed up national cancer statistics showing that men are more likely to develop the most aggressive type of brain tumour, glioblastoma. However, female glioblastoma patients tend to survive the same disease longer and have cancers that respond better to therapy. Is it genetics? Is it hormones? Or is it something else?
While sifting through all this information, she noticed something strange: the cancers from male patients tended to keep on proliferating during treatment, while women’s tumours tended to stop and wait until conditions had improved. It wasn’t 100 per cent true in every case, but the difference between the sexes was clear enough. Swanson became intrigued and started looking for an explanation.
To get to the bottom of the mystery, Swanson teamed up with paediatric neuroscientist Joshua Rubin and his team at Washington University School of Medicine in St Louis, Missouri. Together, they took an in-depth look at data from thousands more cancer patients, as well as studying brain tumour cells growing in the lab and transplanted into mice. Fascinatingly, they found distinct patterns of genetic alterations, gene activity and response to treatment in brain tumour cells from XY males compared with XX female ones, publishing their findings in the journal Science Translational Medicine in 2019.
This included key differences in genes that were already linked to the chances of survival, like a gene called IDH1. Researchers have previously shown that people whose glioblastomas have alterations or mutations in IDH1 are more likely to have a better outcome from treatment. But Swanson and Rubin found that while female patients with IDH1 mutations in their cancers all had the best survival, there was a much wider variety of outcomes for men with IDH1 mutated tumours in all the clusters, suggesting that there’s some kind of interaction going on at a genetic level between the mutations in the cancer cells and the underlying genetic sex of the body they arose from.
Importantly, the researchers also discovered the same differences in brain tumours from male and female children, proving that they weren’t due to the influence of male or female sex hormones found in adults and strongly suggesting that there’s a fundamental disparity in the genetic programming in cancer cells depending on their sex.
Swanson suspects these differences go all the way back through the evolutionary history of the disease. Perhaps, she suggests, cancer cells of different sexes might use different strategies to survive in the stressful environments induced by treatment. By way of example, she points to the different ways in which male and female foetuses respond to food shortages in the womb – a phenomenon known as foetal metabolic programming. In famine situations, a normal number of female babies are born, but they’re unusually small. But for males, the opposite is true: fewer boys are born but they’re all a normal size.
This makes sense in terms of evolutionary programming: if only a few males of a species are needed to impregnate a much larger number of smaller females, then it’s most efficient to allocate biological resources along these lines when times are tight. In a cancer, the equivalent of a famine would be a stress such as radiotherapy, chemotherapy or the restricted, messed-up blood flow that’s often found in tumours. And therefore, according to Swanson and Rubin’s data, the pattern of male cancer cells growing big and strong versus slow-and-steady female cells in response to treatment seems to be recapitulating this evolutionary strategy right down on a cellular level.
The idea that cancer cells might be acting out a deeper evolutionary programme depending on the sex of their host is fascinating, if more than a little controversial. Her discovery has big implications for personalised approaches to treating brain tumours – not only should oncologists take the presence of particular genetic mutations into account when deciding on a treatment, but they should consider the genetic sex of their patient too. It’s also intriguing to wonder whether or not the same pattern plays out in other types of tumour, especially given that cancer drugs are predominantly tested on male animals.
One further question raised by these findings is what happens with brain tumours in people whose gender doesn’t match their birth sex, particularly those taking cross-sex hormone therapy. Do their cancer cells adhere to the underlying genetic programme encoded in their sex chromosomes, or are there other biological and hormonal factors that come into play? There are fortunately very few of these cases around, but Swanson is now doing her best to recruit trans patients to see how their brain tumours behave, and whether they map onto the typical pattern for one sex or the other.
Since their first discovery in brain tumours, Swanson and her team have gone on to dig deeper into the role of sex differences in health and disease. Their latest review pulls together a huge amount of research showing that there are differences in the immune system, metabolism and development between males and females, as well as differences in a range of illnesses and, of course, cancer. And, of course, we also have to go beyond biological sex to consider the impact of gender on health and healthcare, especially where there are inequalities and discrimination that lead to poorer outcomes for some people compared with others.
But, as highlighted by the discovery that we can’t separate the behaviour of tumour cells from the underlying genetic sex of the person they arose in, it’s important to remember that cancer is still part of the body. There’s a common misconception that cancers are somehow ‘other’ alien beings that are growing inside us, rather than the product of our own tissues. But they’re still cells, however messed up they may be, and they’re still going to do the things that cells do. So, we owe it to everyone, whatever their sex or gender, to understand more about how these rogue cells behave in every body and how best to treat them, to make cancer care better for all.
References:
Sex Differences in Health and Disease: a review of biological sex differences relevant to cancer with a spotlight on glioma – Massey et al (2021), Cancer Letters, doi: 10.1016/j.canlet.2020.07.030
Glioblastoma Study Highlights Sex Differences in Brain Cancer – National Cancer Institute blog, 2019
Sex and gender: modifiers of health, disease, and medicine – Mauvais-Jarvis et al (2021), The Lancet doi: 10.1016/S0140-6736(20)31561-0